[Tim Brown's illustration]
He describes desirability as meeting true human needs and desires, as opposed to the drummed up desires personified in perfume ads. On a global scale, these needs include clean water, adequate diet, good health, education for children, and a safe community.
What does "desirability" mean for EMR users?
Here are a few of my ideas. What ideas can you add?
Basic Needs & Desires for Physician and Nurse EMR Users
Rapid, easy, intuitive documentation
- We shouldn't have to type so much. Voice recognition is nearly there, but not mainstream. Voice capture for transcription embedded into the EMR is spotty.
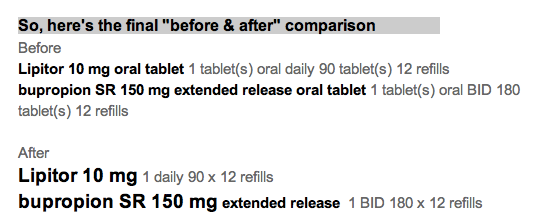
- How about features like "auto-fill" used in e-commerce sites?
- How about "predictive fill" as we see now in Google's predictive search phrases as we start to type?
Smart displays of key information for the task at hand
- The information ought to be visible at a glance.
- No navigation should be needed.
- All the cognitive effort should be squeezed out of the information. Don't make me do mental math. Don't make me remember a rule, or a set of normal ranges. Leave my brain to do only the work that the computer cannot do for me.
Foster collaborative decision-making with patients and their families
- In the hospital, acute pain med doses are often negotiated ("That medicine made me nauseated last time. Can I have something else for pain?" or "Can I have a smaller dose, so I'm not so drowsy?") Give the nurse and patient the tools to decide together.
- In ambulatory care, physicians often explain and negotiate items like bone density scans or PSA blood tests. The guidelines recommend counseling for edge cases, like the most recent guidelines from the USPSTF for mammography for women age 40-49. Give physicians counseling tools that help patients (and doctors, for that matter) understand comparative risks. We do a poor job of that currently.
Enable user-level configurability
- Novices have different needs from more experienced clinicians.
- User preferences change over time. We learn. Make it easy to find and change preferences. Currently, these prefs are buried deep and are widely scattered.
How will these changes happen?