Most clinicians I know suffer from "alert fatigue". I don't mean they feel tired from too much caffeine.
I mean, they are tired of EHR software crying wolf with too many drug interaction warnings. Embattled users simply dismiss all drug interaction warnings without reading them. Mild or theoretical interactions should be suppressable by individual user preference, as a default setting.
This is a significant patient safety issue.
If I am relying on my software to warn me about serious drug interactions, then the warnings about milder or dubious interactions are annoying, distracting false alarms. I need to be aware of serious interactions, so I can adjust therapy.
Here's another problem: I get warned that drug A interacts with drug B. I dismiss the warning. Then I immediately get warned that drug B interacts with drug A. I know that!
Worse yet, if I then change the dose of drug A, I get warned all over again. We need smarter systems now, geared to what fallable, imperfect, tired human users need, and geared to keeping patients safe.
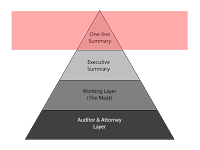
Here is a modest proposal of a way to display drug interactions.
Note that the key findings are in the middle, the drug names are prominent, the severity level is great big number, and user pref settings are right there.